The National Health Service (NHS) Long Term Workforce Plan published in Summer 2023 will impact not only on England’s public healthcare sector but also on the independent healthcare sector. The Plan signals a shift towards a more generalist NHS workforce, with expanded training places and more routes into training and employment over the medium term. With its key priorities being to “Train, Retain and Reform”, it represents a modest attempt to ensure the NHS’ sustainability over the long-term. By targeting a number of straightforward objectives which the NHS have been calling for over the last decade—creating more training places and modernising the NHS pension scheme to boost staff retention—there are few who would disagree with the Plan, but it may be a case of ‘too little, too late’. In this piece, Marwood analyses the potential impacts on England’s health and care workforce and identifies the key takeaways for investors considering assets in this market.
Planned Changes To The NHS Workforce
England’s NHS has been suffering from a staffing crisis since before the Covid-19 pandemic began in 2020. The problem is so persistent that future staff shortfalls have been predicted to exceed 570,000 by 2036. To combat both the current and future staffing issues for the country’s health system, the long-awaited NHS Long Term Workforce Plan was published in June 2023. The Plan sets out to create a sustainable environment for NHS staff and in doing so, to improve the overall number and quality of clinically trained professionals.
Although the Plan sets out lofty ambitions – a reduction in staff shortfalls by 2028, approximately 3% growth in the total workforce – with a higher proportion of new joiners from domestic routes– the plan is at least realistic in recognising that these objectives will take time.
Increasing training numbers to record levels, retaining existing staff, and reforming the NHS workforce to be more flexible and dynamic in its skills, are anticipated to take over 15 years to achieve. With this longer-term view, it is expected that refreshed projections will be published every two years to track progress and align with changes to the landscape.
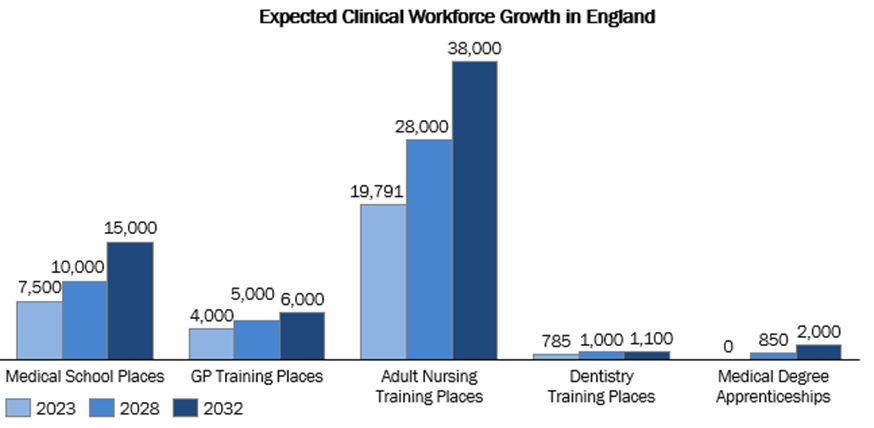
Source: NHS Workforce Plan, 2023
Increased Training Spaces For Healthcare Professionals
As part of the Plan’s unveiling, the Government has pledged to invest more than £2.4 billion to fund the expansion of training places over the next five years. To grow the workforce, the NHS is seeking to significantly expand domestic education, training, and recruitment.
The ambitions for this are significant and include doubling the number of medical school training places from 7,500 to 15,000; increasing the number of GP training places by 50%, increasing adult nursing training places by 92% to 38,000; providing 22% of all training for clinical staff through apprenticeship routes; expanding dentistry training places by 40%, and introducing medical degree apprenticeships with pilots to begin in the next two years by 2031/2032.
Within this, the Plan emphasises lesser reliance of international recruitment and temporary staff. Presently, 25% of the NHS’ workforce is international. Ove the next 15 years, this is expected to drop to less than half of what it is currently. Although this Plan would help the NHS to build up its workforce, it may not last the full 15 years. This is because the £2.4 billion to fund expansion of training places within NHS is only available over the next five years, with funding for the latter decade of the 15-year plan in limbo.
Further, reports from the Royal College of Nursing have cited inadequate pay, unsafe working conditions, and shortage of resources as main reasons as to why NHS staff are currently leaving the NHS. In this regard the Plan is inadequate as it does not acknowledge the key issue of wages, which concerns a broad spectrum of clinical staff as seen in the wave of strikes over pay in the past year.
Ultimately, the conspicuous absence of a Plan to increase wages in the NHS may mean that the Plan fails to solidify retention among existing NHS staff. It may also put future clinical staff off a lifelong career in the NHS. For independent providers this may be an opportunity to use competitive wages and benefits such as work-life balance to attract healthcare professionals.
A Future Of Generalists
In its focus to reform the clinical workforce, the Plan focuses on building up generalists with core skills to care for patients with multimorbidity. This includes increasing the proportion of NHS staff working in primary and community care, expanding existing programmes on generalist approaches, shortening medical degrees from 5/6 years to 4 years, and introducing a ‘earn while you learn’ model. Although the Plan included scant details about the funding to make these shifts happen, if successful, it could provide a much-needed influx of generalist healthcare professionals to the NHS.
A new stream of generalist healthcare professionals may favour independent providers. With the NHS training a new cohort of professionals with more flexible clinical skills and a broader approach to clinical practice, independent providers may find a larger pool of skilled generalists to recruit from over the medium-term.
Modernising The NHS Pension Scheme To Promote Retention
Under the Plan, the Department of Health and Social Care will introduce reforms to the legacy pension scheme in 2023/2024, giving staff the option of partially retiring, or allowing retirees who wish to return to work to continue building their pension and remain in the workforce longer. In this way, the Plan hopes to build on the pension tax reforms announced in the 2023 Spring budget. The changes would help by modernising the NHS pension scheme to allow for flexible work opportunities for prospective retirees.
While these changes may incentivise doctors to continue NHS work for longer, it may also help enlarge the pool of staff that independent providers can retain and recruit from.
The Future Of Workforce Under A Potential Labour Government
With the UK general elections expected sometime before 2025, it is important to consider what would happen to the current plan following a potential Labour Government win. The good news for the sector is that it is broadly expected that this would be retained. Labour have confirmed their commitment to follow through with doubling the number of medical school places to 15,000 a year, and creating 10,000 more nursing and midwifery clinical placements each year.
However, as Labour’s ‘Plan to Protect the NHS’ alludes to, they may also seek to go further, by providing a more significant expansion of the NHS workforce and introducing a new model of care. One of the fundamental differences for workforce under a potential Labour government is due to the Party’s commitment to produce independent projections of staff numbers needed to ensure the workforce is fit for a future. Another key difference is the commitment to working with health staff and their trade unions to review existing training pathways and explore new entry routes to a career in the NHS. However, even Labour have publicly recognised that tax treatment of doctors’ pensions has discouraged some clinicians from continuing in the workforce, so it is unlikely that the plans to address these retention issues would be shelved.
Conclusion
The actions set out in the NHS Long Term Workforce Plan are positive for independent healthcare providers. The Plan has some concrete goals for enlarging the workforce over the medium-term, with changes around NHS pensions likely to increase the number of clinical staff who continue to work following retirement. This is likely to mean that over the short- to medium-term, some of those who would have otherwise retired are likely to continue to form part of the healthcare workforce, whether that is through NHS, or independent sector employment.
Over the longer term, limited funding for training and lack of resolution on wages–key factors to NHS recruitment and retention – may mean the Plan’s implementation is uncertain. Nevertheless, the outlook for workforce considerations is just a little bit brighter for the independent healthcare sector because of these policy developments.
About the Authors
Rosa Juarez is a Director of UK and European Healthcare Advisory at the Marwood Group. Ms. Juarez has worked on a range of projects across health and social care in the UK and major European countries, providing insights on regulatory, reimbursement and policy outlook for investor clients. Prior to joining the Marwood Group, she held senior management positions within England’s National Health Service, with key responsibilities including strategic, operational, and financial planning. Ms. Juarez holds a Master’s degree in International Health Policy from the London School of Economics and Political Science
Dr Vikas Yadav is a Director of UK and European Healthcare Advisory at the Marwood Group. He started his career as an Orthopedic surgeon practicing in India and the UK NHS for 10 years before making a switch to consulting. He has assisted dozens of private equity clients exploring healthcare-related assets. In his last role before joining Marwood Group, he was a Senior Manager in Aetna International’s Population Health business leading strategic projects, business development and marketing. Dr. Yadav holds an MBBS and Master of Surgery degree in Orthopaedics from Banaras Hindu University in India and an MBA from INSEAD in France.
Ting Yi Wong is an Analyst at the Marwood Group. In her role, Ms. Wong has worked across projects undertaking quantitative and qualitative research and analysis of UK and international health and social care data and is able to provide in-language research for Mandarin projects. Ms. Wong achieved her undergraduate degree in Biomedical Science (Hons) at the University of Dundee in 2020 and an LLM in Medical Law and Ethics in 2021 at the University of Edinburgh. Ms. Wong also has previous experience working in medical communications for projects in the UK and Asia-Pacific region.